A strong response to antimicrobial resistance must include tackling TB.
Antimicrobial Resistance
Antimicrobial resistance (AMR)—which occurs when microorganisms no longer respond to the drugs designed to treat them—is becoming one of the defining health issues of our time. The threat posed by “superbugs” to public health, safety, and the global economy is staggering.
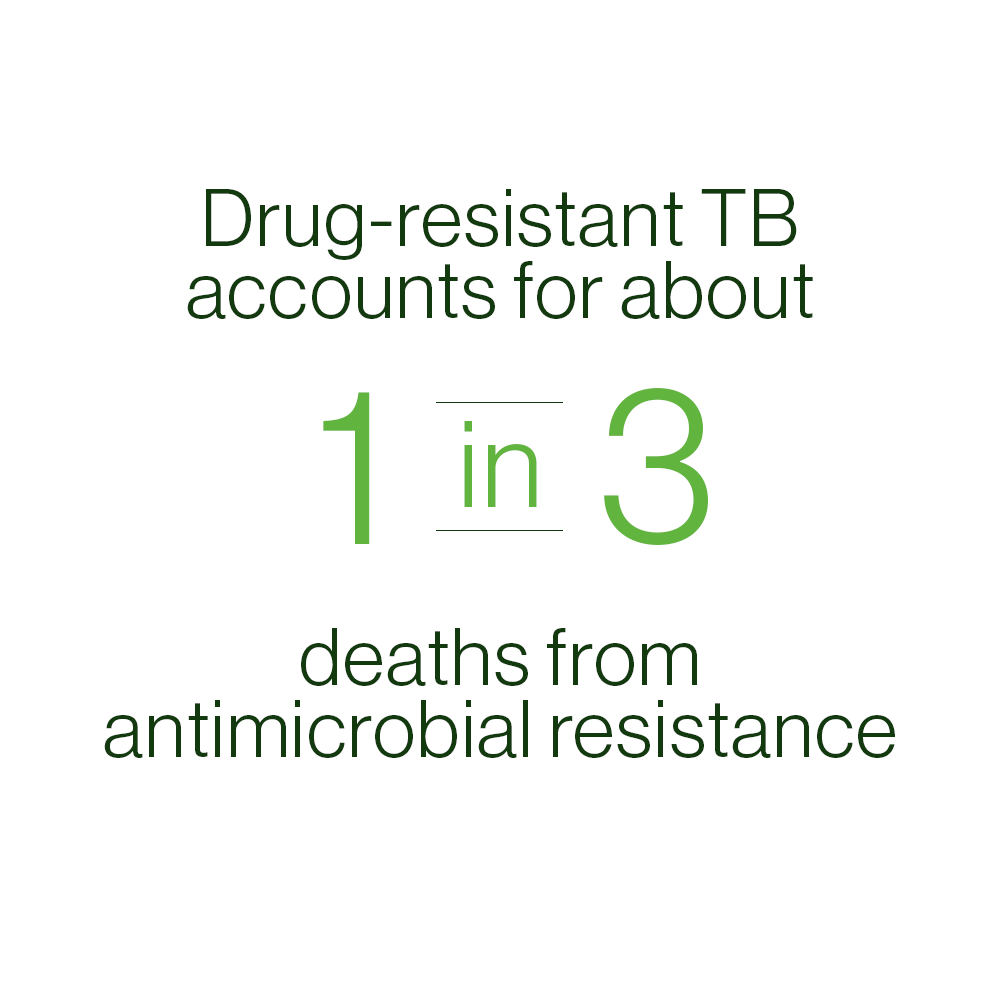
While AMR is often associated with hospital-based infections, like MRSA (methicillin-resistant Staphylococcus aureus), about 29% of deaths caused by antimicrobial infections today are due to drug-resistant TB. In fact, the grim projections forecast for the “post-antibiotic age” are already a reality for many countries and patients who are experiencing the human and economic toll of multi-drug resistant (MDR-) and extensively drug-resistant (XDR-) TB.
This is one day of traditional treatment for drug-resistant TB.
Today’s treatment can last two years or longer, is highly toxic, and ineffective.
“The advent of a better treatment regimen for MDR-TB would by itself quickly start to save a large number of lives, with more than 20,000 deaths being averted every year within three years of the new treatment’s introduction.”
A Growing Threat

MDR-TB:
MDR-TB, multidrug-resistant TB, is defined by resistance to the two most commonly used
drugs in the current four-drug (or first-line) regimen, isoniazid and rifampin. It is the result
of interrupted, erratic, or inadequate TB therapy, and its spread is undermining efforts to control
the global TB epidemic. Drug-resistant TB develops when the long, complex, decades-old TB drug
regimen is improperly administered, or when people with TB stop taking their medicines before the
disease has been fully eradicated from their body. Once a drug-resistant strain has developed, it
can be transmitted directly to others just like drug-susceptible TB. There are more than 400,000
cases of drug-resistant TB each year. MDR-TB is such a global health threat because the medicines
are very expensive, take years to work, and ultimately inadequate to stop the disease and its spread.
Antimicrobial resistance is dangerous in all its forms, however, MDR-TB yields a global threat to
health and economic development. A recent report from a UK parliamentary group stated over the
next 35 years, multidrug-resistant tuberculosis will kill 75 million people and could cost the
global economy a cumulative $16.7 trillion — the equivalent of the European Union’s annual output.

XDR-TB:
Extensively drug-resistant tuberculosis, or XDR-TB, is a strain of tuberculosis, airborne and infectious, that is resistant to four commonly-used anti-TB drugs. Until the US FDA approval of pretomanid as part of the BPaL regimen, there was no reliable cure for XDR-TB. XDR-TB has been confirmed in 127 countries around the world and represents about six percent of all MDR-TB cases. XDR-TB is emerging as an extremely deadly and costly global health threat that the world must mobilize rapidly to tackle.
Drug-resistant TB is a continuing threat. In 2022, 410,00 cases of drug-resistant TB.
—World Health Organization, 2023
Dire Costs
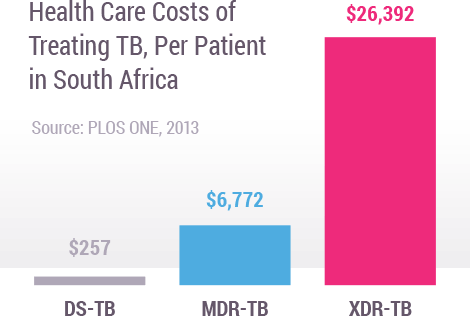
When infections become resistant to first-line drugs, more expensive therapies must be used to treat them. Lengthier treatment, often in hospitals, substantially increases health care costs as well as the economic burden on families and societies. The cost of treating a single case of MDR-TB or XDR-TB can be thousands of times more expensive than treating drug-sensitive TB. For example, in South Africa, drug-resistant TB consumed about 32% of South Africa’s US$218 million national TB budget (2011), despite the fact that it only accounted for about 2% of all TB cases.
Inadequate Treatment
Today, treatment for drug-resistant TB is long, toxic, complicated and expensive.
6
Months
Months
Injections
1/day for at least 6 months.
9-24
Months
Months
Pills
12-24/day for as many as 24 months.
6-24
Months
Months
IV Infusions
2/day for 6-24 months.
14,000
Pills
Trillion Dollars
It takes 14,000 pills to treat one patient with drug-resistant TB.
Our Pipeline
To overcome treatment challenges, TB Alliance is developing the largest pipeline of new TB drugs in history.