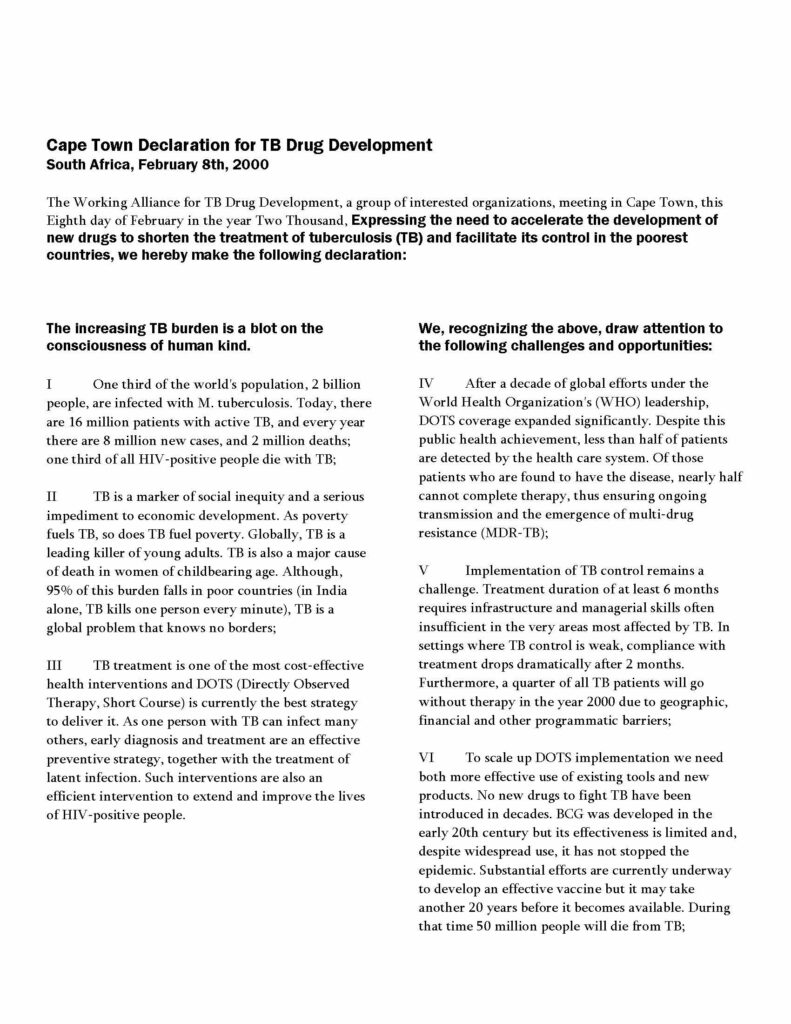
February 8th marks the 25th anniversary of the signing of the Cape Town Declaration, which birthed TB Alliance. Throughout the year, we will be sitting down with leaders and visionaries in the TB space and learning from the past, analyzing the present, and charting the future of TB research. It is fitting that the first installment of this series would feature founding TB Alliance Board Member Ariel Pablos Mendez, who touches on the impetus for TB Alliance’s creation, how success has sharpened our understanding of what’s possible, and why the core challenges and vectors of impact remain similar. Read more from our discussion below.

Ariel Pablos-Mendez accepts an achievement award for his service on TB Alliance’s Board of Directors
Twenty-five years ago, when TB Alliance was being formed, what were some of the biggest challenges with TB treatment? What were the main obstacles to solving them?
The main challenges in TB treatment were three. First, multidrug-resistant tuberculosis (MDR-TB) was emerging as a serious problem. Second, we had 8 million cases, but few of them actually completed treatment since they were required to take six to nine months of treatment, which was too long. Third, we were fighting TB with drugs from the ’50s—fifty years with no new tuberculosis drugs because markets weren’t strong enough to attract industry interest, which had shifted to noncommunicable diseases.
WHO did a fantastic job expanding DOTS, helping to ensure treatment adherence. But its focus on expansion sidelined innovation and R&D. At the Rockefeller Foundation, I saw an opportunity to bring that community together, which led to the Cape Town Meeting in February 2000.
How would you characterize the progress in improving TB treatment over the last 25 years and TB Alliance’s role in achieving that progress?
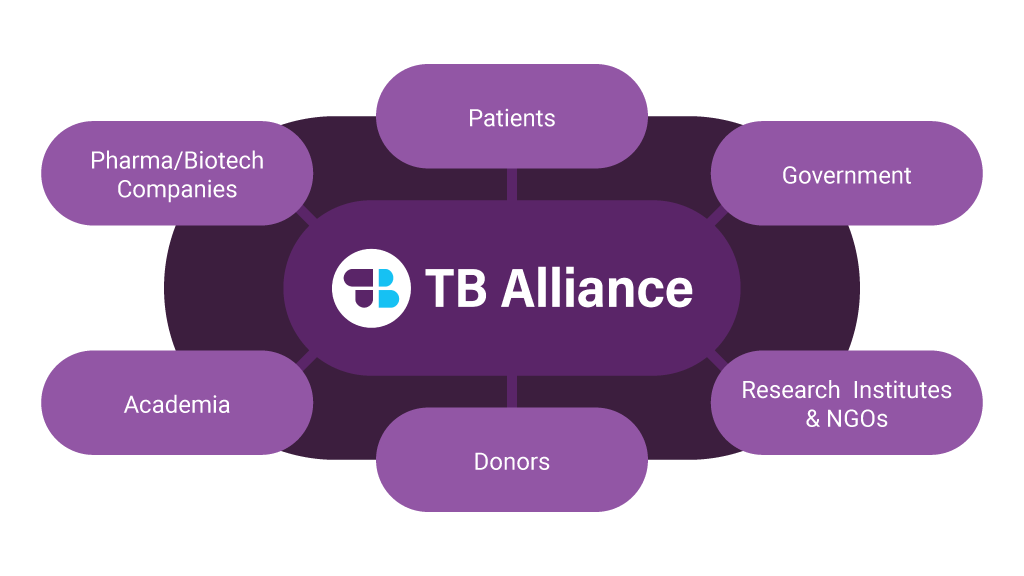
I think it’s been quite fantastic for something that was an experimental model—this new set of public-private partnerships in product development. At Rockefeller, we had been cultivating this approach, first with the International AIDS Vaccines Initiative (IAVI), then with the Medicines for Malaria Venture (MMV) and others. For the Global Alliance for TB Drug Development, I brought in lessons from those initiatives and set it up as the “best in class.”
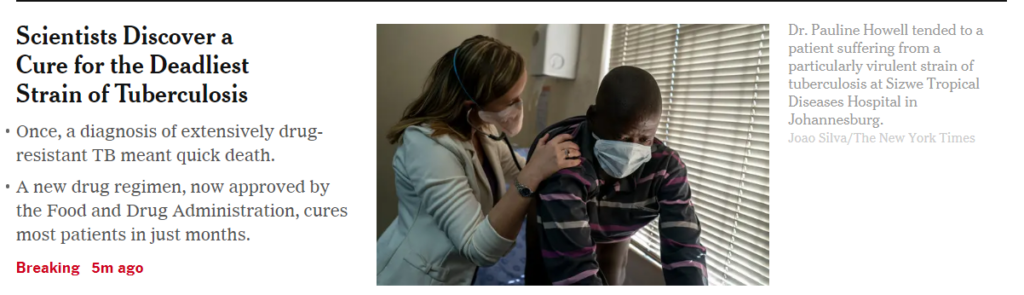
And the TB Alliance team has done a fantastic job—from procuring the right compounds to bringing in the right scientists and working with private sector expertise. The approval of pretomanid for DR-TB was a major success. It probably cost more than we had in mind to develop the first drug – but it delivered not just a new drug, but a new regimen. More importantly, TB Alliance now has a pipeline, and the broader TB R&D space is energized, with many efforts joining – rather than competing – with the Alliance.
A lot has been achieved, which brings a certain stability and helps to enable exploration of areas like leprosy and other non-tuberculous mycobacterium. I told my wife 25 years ago, after the birth of TB Alliance, that I didn’t need to do anything else for the world. I feel very proud of that. The model of public-private partnerships in product development for global health has been an incredible success.
What do you think are the biggest differences about working in TB product development in the early days of TB Alliance and working in TB R&D now?
Well, obviously success – that makes a big difference. From a time of neglect and need, to a time of a lot of engagements, resources, and results and hope for even bigger achievements – these are things that are very much the difference. There was no ecology really, there were isolated efforts of champions at the NIH, in the industry, some universities, but they just didn’t have enough of the threshold to get traction. And so now we have traction, and we have an ecosystem of many other efforts and partnerships and new institutions that are gearing up to address the mission of the Global Alliance for TB Drug Development. And so, to me, that’s a double success. Not only has the Alliance itself delivered, with approval of new drugs and reaching patients in over 100 countries, but also many others join in the work.
Looking ahead, what do you think are the highest priorities and biggest potential breakthroughs for TB Alliance over the next five years?
The key things remain the same as 25 years ago, but now we have a sharper sense of possibilities and portfolios to back it up. We need to continue developing and fine-tuning drugs for multidrug-resistant tuberculosis, but more importantly, treatments that are blind to drug resistance—new medications that can treat patients regardless of resistance.
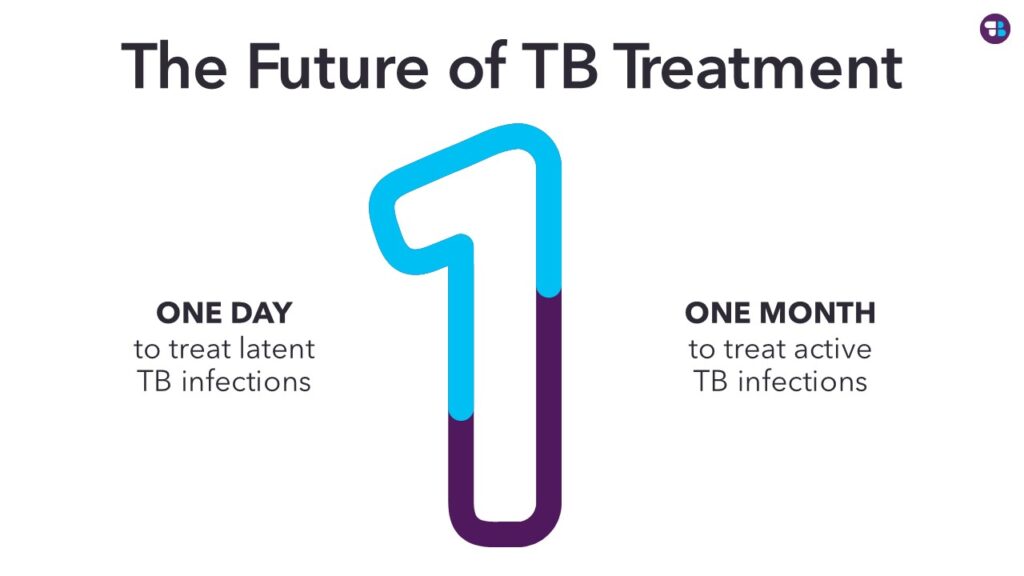
Treatment duration has always been a challenge. For MDR-TB, we’ve gone from 18 months of toxic, injectable, and only partially successful drugs to six months, oral, less toxic, and highly effective treatments. But for regular TB, reducing treatment from six months to one month would be a revolution, and the Alliance has embraced that ambition.
Another priority is preventing TB by treating those infected but not actively ill. Working toward a one-day treatment for latent infection—potentially injectable similar to a vaccine—is a great aspiration.
Breakthroughs are coming. The ambitious goals of resistant-blind treatment, one-month TB treatment, and one-day prevention are now possible. The strategy development process aligns well with where our technical leaders see the possibilities.
So, 25 years ago, we had almost nothing, but at the same time, just dreaming of having one drug, one new drug, was like an incredible dream. To now, be able to be so bold and ambitious as to imagine a one-month treatment, a one-day prevention and resistant-blind regimens, those are incredible dreams we have now. Many are excited, and I believe we’ll be there by the end of the decade.